OsseoMatrix™: A Bioengineered Porous Architecture Bridging Biology and Engineering for Precision Bone Repair
Advancing Orthopedic Care Through Biomimetic Structural Design

OsseoMatrix™: A Bioengineered Porous Architecture Bridging Biology and Engineering for Precision Bone Repair
Advancing Orthopedic Care Through Biomimetic Structural Design
The use of synthetic bone substitutes remains a critical challenge in modern orthopedic surgery. Despite advancements in material science and surgical technology, conventional bone implants continue to face limitations—particularly in their ability to integrate seamlessly with native bone tissue. These limitations often result in mechanical instability, prolonged patient recovery times, and suboptimal long-term outcomes.
In response, contemporary clinical strategies have shifted toward designing implants that closely mimic the structural and functional properties of natural bone. The goal is not only to enhance implant stability but also to promote tissue regeneration and reduce long-term complications.
OsseoMatrix™ represents a major innovation in this domain. Engineered using a Triply Periodic Minimal Surface (TPMS) porous architecture, OsseoMatrix™ enables controlled mechanical loading, uniform stress distribution, and an ideal microenvironment for bone cell proliferation. This biomimetic scaffold significantly accelerates bone healing, enhances fixation stability, reduces recovery time, and minimizes the risk of long-term implant degradation.
More than a porous structure, OsseoMatrix™ is a convergence of engineering precision, biological compatibility, and advanced manufacturing. It embodies the principles of personalized medicine by enabling patient-specific orthopedic interventions—an emerging standard in next-generation surgical care.
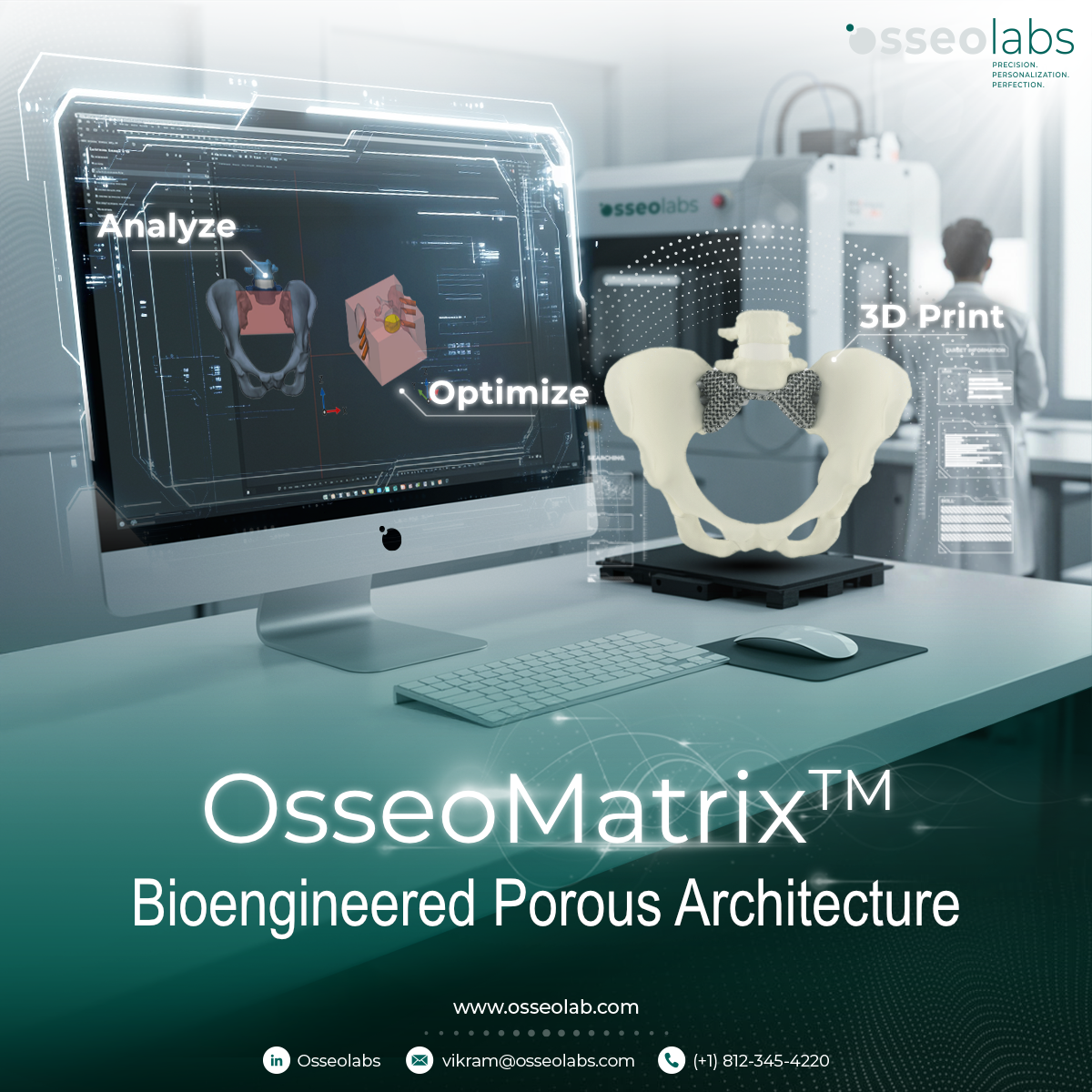
How OsseoMatrix™ Works
Over the past decade, orthopedic implant design has evolved from simple strut-based lattices to highly sophisticated porous structures. Triply Periodic Minimal Surface (TPMS) designs exhibit continuous, symmetric geometries with a mean surface curvature of zero. These features ensure optimal stress distribution, enhanced fluid permeability, and nutrient transport—mimicking the trabecular bone architecture found in human anatomy.
Studies have demonstrated that TPMS-based scaffolds are highly suitable for synthetic bone applications, enabling precise control over critical parameters such as pore size, wall thickness, Gaussian curvature, and relative density. These factors directly influence mechanical strength and osteoconductivity—key determinants of successful bone regeneration (Poltue et al., 2021).
OsseoMatrix™ leverages these structural advantages by employing full TPMS geometry, achieving an optimal balance between mechanical integrity and biological integration. Further enhanced through the principles of Functionally Graded Structures (FGS), OsseoMatrix™ incorporates variable porosity and wall thickness to better emulate the stress dispersion of natural bone. Research by Karuna et al. (2022) indicates that such gradients reduce stress shielding, lower stress concentrations, and improve long-term implant-tissue integration.
Importantly, the use of graded structures also aligns elastic modulus and permeability with physiological conditions—minimizing the risk of implant fatigue, microfractures, and mechanical mismatch over time.
Designed for Clinical Use, Optimized for Patient Recovery
OsseoMatrix™ is more than a porous implant—it is a patient-specific solution tailored to anatomical and clinical needs. Each design is customized to the individual, ensuring improved fit, enhanced safety, and optimal conditions for bone regeneration.
By enabling the implant to conform to the patient's anatomy and biomechanical profile, OsseoMatrix™ contributes to a more natural functional recovery. Patients benefit from shorter rehabilitation periods, improved implant longevity, and a lower incidence of inflammation or device failure—common drawbacks of traditional implants.
The Future of Bone Surgery with OsseoMatrix™
Implants manufactured using OsseoMatrix™ technology are fully customizable to match each patient’s anatomy and loading requirements. The ability to withstand biomechanical forces while promoting natural tissue ingrowth enables surgeons to offer care that is both technically superior and clinically personalized.
OsseoMatrix™ becomes even more powerful when integrated with OsseoVision™, OsseoLabs’ proprietary AI-powered surgical planning platform. Using patient CT data, OsseoVision™ enables surgeons and engineers to co-develop implants with pinpoint precision. The AI-driven system optimizes structural parameters to create designs that maximize both performance and biocompatibility.
A Vision for Precision and Personalization
Driven by the vision to “Provide perfect surgical solutions through personalization and precision,” OsseoLabs is redefining the future of orthopedic surgery. OsseoMatrix™ is not only advancing the quality of patient care—it is setting a new benchmark for safety, efficacy, and design innovation in the global medical device landscape.
As personalized implants become the new standard of care, OsseoLabs stands at the forefront—empowering surgeons with transformative tools and giving patients access to better, faster, and safer healing.



.JPG)
.jpg)

